What keeps venous leg ulcers from healing?
Chronic venous insufficiency can cause valves in the leg veins to stop working properly. These damaged veins may lead to complications such as varicose veins, pressure, swelling and skin breakdown with open sores known as venous leg ulcers (VLU).
Typically occurring on legs or ankles, VLUs may be hard to identify, especially if a person’s medical history is unclear. If not assessed correctly, inadequate treatment may delay healing. Even after a VLU has been identified, other challenges can prolong healing times, including:
1. Lack of proper skin care, often a result of patients and caregivers not using the right products consistently
2. Patient non-adherence due to misunderstandings, as well as physical, psychological and other hardships
3. Risk of infection from biofilm in chronic wounds
Together, we help clinicians and patients overcome venous stasis challenges with evidence-based best practices and the right system of products.

Up to 50% of VLUs remain unhealed at 6 months¹
Proactively treat and manage VLUs with a 3-part approach
Venous leg ulcers are difficult to heal, and studies show that 72% recur within 5 years¹. That’s why it’s important to support caregivers and patients with tools and strategies that address intact skin, improve blood flow in the veins and reduce risk of infection.
Proper skin care
Using a complete system of skin care products consistently makes it easier to maintain skin integrity.
Effective compression
Studies show the right amount of consistent compression helps reduce recurring wounds.
Advanced wound care
Innovations in wound dressings take a proactive approach to fighting biofilm in chronic venous leg ulcers.
Protect intact skin from breakdown
While managing venous ulcers, it’s important to maintain proper skin care. Use nutrient-rich skin care products and follow these important steps:
- After removing compression wraps, wash the leg thoroughly, rinse and dry completely. This cleansing routine gives you an opportunity to inspect the wound as well.
- Gently moisturize intact skin around the wound.
- If there’s drainage, use a moisture-barrier product, as fluids can cause damage to skin around the wound.

Keep skin moisturized
Moisturize with 12.5% dimethicone to help soothe fragile skin and resist moisture loss.

Create a strong barrier
Build lasting protection with a paste that contains an effective combination of zinc-oxide and white petrolatum.
Control the underlying venous disease
Compression therapy helps blood move, reduces pressure in the veins and decreases swelling. That’s why it’s considered the gold standard for managing chronic venous insufficiency symptoms and venous leg ulcers.
But people sometimes find compression uncomfortable or disruptive to their lives, and they give up. That’s when VLUs can recur. How can you help ensure compression is successful?
- Choose a compression device that’s effective, easy to apply, breathable and comfortable.
- Educate patients on the importance of self care.
Keep in mind, if a person complains of pain with compression, stop and reassess the situation. You could be dealing with an arterial wound, which would not be right for compression.
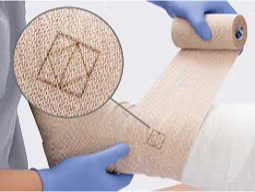
Achieve accurate compression
A 2-layer system with accuracy indicators makes it easier for clinicians to achieve optimal pressure.

Encourage patient compliance
At-home compression devices with AccuTabs are more comfortable, simple to apply and help improve quality of life.
Improve healing time with the right tools
Treating a hard-to-heal venous ulcer starts by removing wound exudate. Look for an advanced wound dressing that effectively absorbs drainage. If there’s no progress after about two weeks, try gentle debridement with a concentrated surfactant, which can work under the dressing.
Remember that biofilm can delay chronic wound healing, so be armed with a hard-working antibacterial foam dressing.

Reduce exudate
Create a strong, absorbent and conformable gel with a dressing that contains chitosan.

Manage infection
Improve infection management through slow-release iodine within the wound dressing.
Experience our products for yourself: Request a sample
Simply complete this form and a Skin Health specialist will contact you soon to coordinate your no-cost sample.

Learn more about caring for venous stasis
References:
- TTreadwell, T., Sabolinski, M. L., Skornicki, M., & Parsons, N. B. (2018). Comparative Effectiveness of a Bioengineered Living Cellular Construct and Cryopreserved Cadaveric Skin Allograft for the Treatment of Venous Leg Ulcers in a Real-World Setting. Advances in Wound Care, 7(3), 69–76. Available at https://doi.org/10.1089/wound.2017.0738




